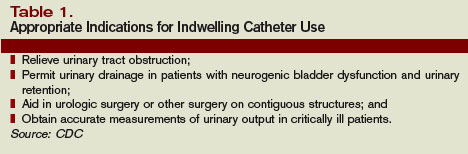
To prevent urethral complications catheters with a smaller size 1214 F for men and 1416 F for women 48 as large a lumen as possible and smaller 510 mL selfretaining balloons are recommended to reduce the pressure effect on urethral surface and the bladder neck and to minimize obstruction of the urethral gland in men. The continuing popularity of FCs is demonstrated by the fact that between 16 and 25 of hospitalized patients have an indwelling Foley catheter during their hospital stay1 2 FCs have associated risks the most recognized being the propensity of the catheter system.
 Complications Of Foley S Catheter Youtube
Complications Of Foley S Catheter Youtube
A Foley catheter is a sterile tube that is inserted into your bladder to drain urine.
Foley catheter complications. Check out a case where a man bled to death from forceful urinary catheter. Urine leaks from or around the catheter tubing or drainage bag. I am very familiar with current standard of care for Foley catheter placement and management especially for inpatients and catheter related complications such as trauma related complications and catheter associated UTIs CAUTIs.
What are the potential complications of urinary catheters. However elderly people and those with a permanent injury or severe illness may need to use urinary catheters for a much longer time or permanently. The tip of the catheter has a small balloon filled with solution that holds the catheter in your bladder.
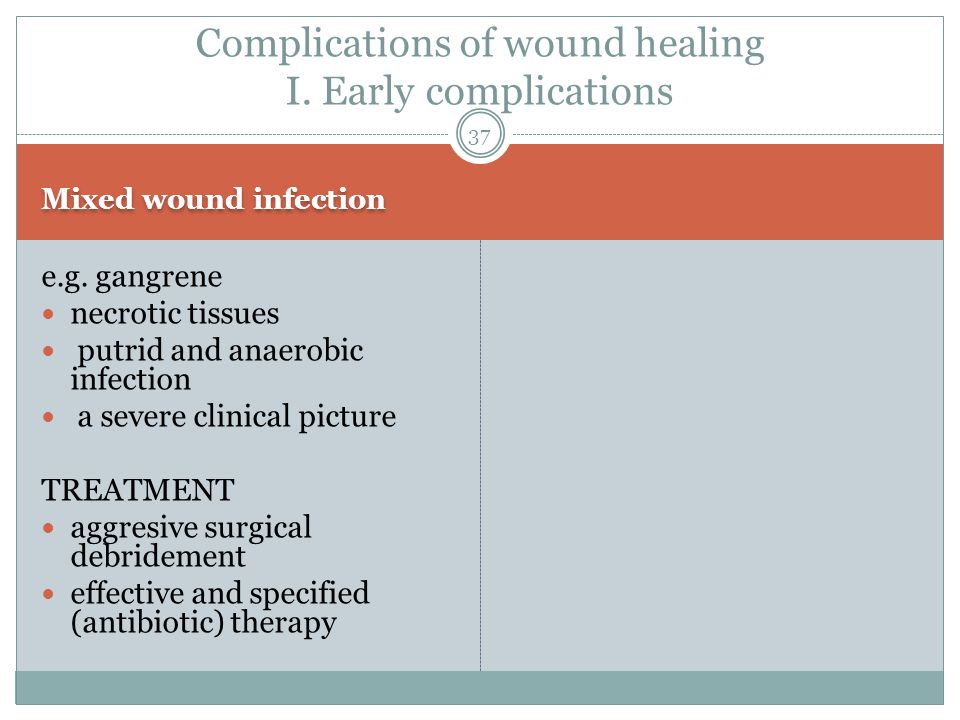
Indwelling urinary catheters have been an integral part of medical care since the invention of the Foley catheter in the 1930s. Although symptomatic urinary tract infection and asymptomatic bacteriuria are frequently discussed genitourinary trauma receives comparatively little attention. The Foley catheter may introduce an infection into the bladder.
Foley catheters cause a variety of harms including infection pain and trauma. You have questions or. Repeated burst Foley catheter balloon with peristomal leakage n 4 lumen blockage n 1 and catheter migration resulting in small bowel obstruction n 4.
The risk of infection in the urine increases with the number of days the catheter is in place. Several complications with IC have been described however including urinary tract infection genital infection urethral bleeding urethritis urethral stricture and bladder stones. Get Results from multiple Engines.
You see a layer of crystals inside the tubing. Moreover patient tolerance is often limited. According to an article in BMC Urology indwelling urinary catheters are the leading cause of healthcare-associated urinary tract.
The closed drainage system has accidently come open or apart. Complications occurred in nine 426 patients. Allergy or sensitivity to latex.
One of the most common and severe complication that occurs with urinary catheters is a UTI referred to as a catheter-associated urinary tract infection or CAUTI. A CAUTI can lead to urosepsis and septicemia Infections are common because urethral catheters inoculate organisms into the bladder and promote colonization by providing a surface for bacterial adhesion and causing mucosal irritation. Ad Search For Relevant Info Results.
Urethral Injury - Urethral injury due to trauma is a common complication associated with Foley catheters especially if the catheter is inserted forcefully or roughly. All complications were successfully managed with tube replacements. Complications of Balloon Tamponade Foley catheters are associated with the same complications as nasal packing.
A significant urethral injury can even cause death. It is also called an indwelling urinary catheter. To prevent these complications patients should be well instructed on the technique and the.
You have a rash or itching where the catheter tube is secured to your skin. Get Results from multiple Engines. This article is dedicated to the matters of change and negotiation regarding complications prevention of Foley Catheter use in surgical patients.
If the balloon is opened before the Foley catheter is completely inserted into the bladder bleeding damage and even rupture of the urethra. It identifies the target audience various stakeholders and describes the change and negotiation strategies that could be implemented in this situation and offer a proposed communication plan for the. Complications arising soon after catheter implantation are frequently related to the procedure itself congenital anatomic abnormalities andor to increased intra-abdominal pressure IAP generated by infusion of dialysate into the peritoneal cavity1.
Medical Complications of Catheter Use Most catheters are necessary until you regain the ability to urinate on your own which is usually a short period of time. However they are more common eg in the case of respiratory compromise and they may be more severe. Ad Search For Relevant Info Results.